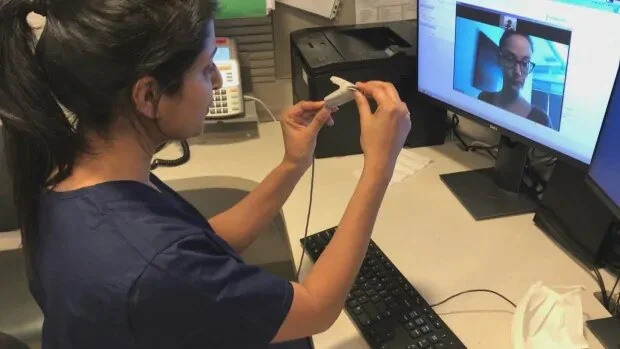
Canadians embraced virtual health-care options like phone or video appointments during the COVID-19 crisis, according to a new poll released by the Canadian Medical Association (CMA).
The survey released on Monday suggested 47 per cent of Canadians have used “virtual care” such as calls, email , texts or video during the pandemic. Of these, 91 per cent said they were very satisfied with the experience.
“Canadians were forced to physically distance, to isolate themselves, to stay at home,” said CMA president Dr. Sandy Buchman of the COVID-19 restrictions. At the same time, virtual care increased and the CMA wants to see it expand.
“We need to seize the moment. We need to find if there’s a silver lining on this,” Buchman told CBC News.
Buchman, a palliative care physician for people who are homeless in Toronto, called for improved access to cellphone and high-speed internet service in rural, remote and Indigenous communities — while addressing issues including quality of care and privacy.

Buchman said he wasn’t surprised by the survey’s findings, given how commonly Canadians bank and shop online and what he heard anecdotally as visits to medical offices and emergency departments declined.
In Canada, questions include whether people who did not access health care virtually during COVID-19 in fact didn’t need to or didn’t know how to do so.
Respondents were asked about routine care, like renewing regular medications for asthma or a heart condition; basic needs such as addressing new symptoms; and complex care like for cancer or multiple diseases.
Most still prefer in-person visits
Of those surveyed who needed advice during the pandemic, 34 per cent reached their doctor by phone. About 10 per cent saw a doctor face to face, six per cent went to a walk-in clinic and five per cent to an emergency department.
Another seven per cent used their provincial telehealth service, six per cent used videoconferencing, six per cent used a private virtual health provider and four per cent used text or email.
Looking ahead, about 58 per cent said they’d prefer to initially reach a doctor in person compared with 20 per cent who would prefer a phone call, 14 per cent who would choose videoconference and eight per cent for email or text.
Dr. Iris Gorfinkel, a family physician in Toronto, says for people who are young, healthy and in higher socioeconomic groups, a phone likely works well to connect with a physician.
“Video conferencing I think would be very difficult for the most vulnerable patients, older patients to do,” said Gorfinkel who is currently reaching most patients by phone. She wasn’t involved in the poll.
“Where do the impacts of the worst health outcomes land? Precisely in that group.”
Other vulnerable populations include those with low socioeconomic status. “You’re hard-pressed to name a condition in which low socioeconomic status is not a predictor,” of poorer health outcomes, she said.
Gorfinkel also worries about missing subtle cues in a phone call, such as if the person shaved, how they smell or if someone says “everything is fine” while a tear runs down the cheek.
Gorfinkel would also like to see research into the full, long-term costs of virtual care. For instance, she now orders more diagnostic tests like X-rays and ultrasounds when a physical exam can’t be done to check a patient’s abdomen for enlarged organs or other problems.
Abacus Data conducted the national poll of 1,800 Canadians for the CMA between May 14 to 17.

Source link
Be First to Comment